Dengue Fever Transmission in Underserved Urban Communities
by Adelaide Loechl, Anthropology
Due to the pressing issue of climate change, infectious diseases like dengue fever have been making a powerful resurgence across the globe. Rising global temperatures have allowed dengue fever’s geography to expand, putting more people at risk for infection. In urban areas of lower socioeconomic status, the burden that dengue fever has placed upon communities is increasingly apparent. This struggle has been exacerbated by the increase in urban populations in tandem with crumbling infrastructures. Lack of governmental support on these issues leads to insufficient housing and poor wastewater management and storage, as well as limited access to healthcare. Communities are left to fight rising infection rates by themselves, while lacking access to the tools that would help them. In order to control the spread of dengue fever and protect underserved communities, public health officials must implement vector control methods such as case tracking, implementing wastewater management systems, educating communities, and developing vaccines.
dengue fever, climate change, socioeconomic status, urban communities, public health, anthropology
Introduction
Upon hearing the term “infectious disease” one may first consider the symptoms, infection rate, and mortality of a disease. While these aspects are important, they do not provide a full picture of a disease. A different and often overlooked set of factors such as environment, socioeconomic status, living conditions and culture are the driving force behind infectious disease spread. When it comes to dengue fever, this angle is crucial. Dengue fever is one of the most elusive viral diseases of the modern day, especially for socioeconomically disadvantaged communities. With control methods in the past failing as well as having no developed vaccine, certain areas of the world fall victim to large numbers of dengue fever infections. The spread of dengue fever in socioeconomically disadvantaged areas is determined by interaction between social and biological elements, directly linked to migration, climate change, and infrastructure issues.
The Yellow Fever Mosquito and Dengue Fever
Originating in Africa, Aedes aegypti is the species of mosquito that is responsible for the spread of dengue fever. This species is a well known vector of mosquito borne illnesses, as it also is responsible for the spread of yellow fever and the zika virus (Kularatne 1). Because of this, it is generally referred to as the Yellow Fever Mosquito (Desjardins et al. 1). What these insects are actually carrying is an RNA virus that is a member of the Flavivirus genus. Other members of this genus include the West Nile virus and of course, yellow fever.
The Yellow Fever Mosquito can carry five varieties, or serotypes of dengue fever (“Dengue Areas of Risk Around the World | CDC”). Not all serotypes are equally dangerous, as the first and second are known to cause more serious infections. Infection via a single serotype leads to immunity from that strain. However, individuals can become infected with multiple strains at one time. In these cases, symptoms will become much worse than if they were infected with a single strain (Desjardins et al. 1).
After the initial bite, an individual will begin to show signs of infection within a fourteen day period. The way in which symptoms present themselves differ. Most people (around 80% percent) who have been infected will never show signs of infection. Those who do will suffer from flu-like symptoms such as a fever, skin flushing, body aches and bone pain. Gastrointestinal issues like nausea and vomiting have also been reported. Serious or untreated infections may cause hemorrhagic fever and dengue shock syndrome, which can be fatal (Kularatne 2).
Dengue Fever and Climate Change
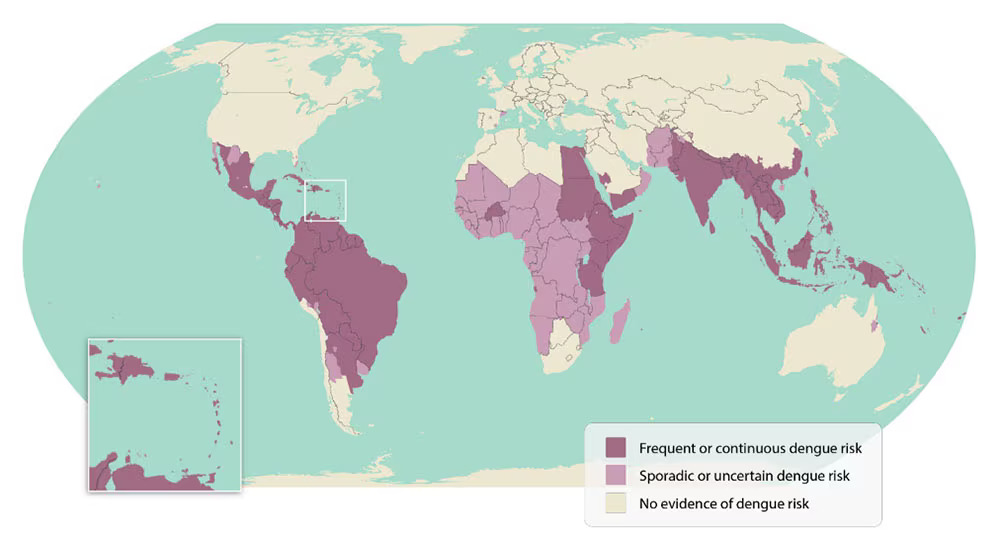
Historically, this disease has been contained to certain areas of the world, as it is climate dependent. In the past, tropical and subtropical environments have proved to be the perfect breeding ground for dengue fever. The Yellow Fever Mosquito requires warm, humid temperatures in order to survive. The ideal conditions for this insect are around 28 degrees Celsius (or 82 degrees Fahrenheit) and eighty-five percent humidity. As a result, most cases have typically been found within southeast Asia, the western Pacific, and South America. Nevertheless, what once was a disease restricted to distinct areas of the tropics is now one of the fastest spreading vector-borne illnesses on Earth. Within the past fifty years, infection rates have skyrocketed to a rate thirty times what they were before. Now, the disease is found in over one hundred countries across the world (Cromar and Cromar 167). The rapid increase in infections begs the question, “What is causing this monumental spread?”. Unfortunately, climate change
plays a role. As global temperatures rise, A. aegypti is able to survive in new areas. Temperature increase is also linked to more frequent bites from infected mosquitos. Mosquito development time has shortened, causing adults to become smaller on average with lower energy reservoirs. This leads to adult females needing to feed more often in order to reproduce, causing the numbers of bites to escalate (Cromar and Cromar 172). Due to this, future predictions of where risk and dengue fever stand are looking bleak. In 1990, only 1.5 billion people were at risk for contracting the disease. Considering population growth and escalating carbon dioxide emissions, it is estimated that 5-6 billion people will be at risk by 2085 (Cromar and Cromar 176). Population growth coupled with climate change stands to further complicate the spread of the virus into areas where the infrastructure is unable to support numbers of infections. In these areas, socioeconomic status plays a huge role in potential exposure.
Urbanism and Class
Unanticipated migration into urban areas is leading to infections spreading faster (Chang et al. 93). Rapid urban growth can be caused by various elements. Individuals of lower socioeconomic status often move to urban areas due to lack of work, lack of resources and as climate change worsens, natural disasters. Those living in poverty are most at risk of experiencing the effects of natural disasters and therefore climate change. Displaced people have few choices but to move towards an urban setting in search of a better life (Chang et al. 94). Unfortunately, a sudden influx of people resulting in urban population booms creates consequences. These consequences include overcrowded and poorly built housing, sanitation issues, and water management problems. Below-standard living conditions where hygiene is not emphasized promotes the resurgence and spread of diseases like dengue fever (Heymann 134).
This spread directly affects socioeconomically disadvantaged areas, as they do not have the infrastructure to protect against infections.
Urban housing infrastructures are struggling to keep up with the new population demands (Chang 98). This creates an urban nucleated settlement pattern in which there are not enough houses for the amount of people living in a certain area. Under these circumstances, multiple families will live under the same roof, finding whatever housing there may be (Whiteford 209). Homes that are over capacity generate more waste, including trash, waste water, and other places where mosquitoes can breed. Lack of air conditioning also encourages humidity and the formation of stagnant water. Furthermore, the housing that is built in economically depressed communities is oftentimes poorly constructed and not well maintained. In these homes, cracks can form in the roof and walls due to water damage and in turn allow
mosquitos to enter. Water that has accumulated in the home can become stagnant, creating the perfect environment for mosquito reproduction. Without government support for housing infrastructures, communities are left to fend for themselves lacking the resources to efficiently address the problem.
Water access and supply is one of the most important infrastructural aspects to consider when it comes to dengue fever. Poor water storage and management is a hallmark of inadequate urban planning due to overpopulation. This occurs because little to no wastewater management systems are implemented in underprivileged areas. With no allocated place to dispose of water, it accumulates in houses, streets and in household goods that have been thrown out. Items like plastic containers, jars, and tires become mosquito breeding sites (Heymann 136). The survival of A. aegypti is dependent on humid areas with warm, stagnant water. While periods of heavy rainfall initially prevent stagnant water from accumulating, they actually result in more infections. Frequent rainfall will initially rid mosquito larvae from water but the aftermath leads to more pools of stagnant water forming, causing new mosquito breeding locations (Chang et al. 97). Additionally, dry periods also contribute to infection rates. During a rainy season water is collected and stored to use during the dry seasons, but many socioeconomically disadvantaged communities do not have the resources to store this water safely (Cromar and Cromar 174). Lack of reliable access to drinking water also imposes a threat. This was shown in a study conducted in northeastern Brazil that focused on how communities navigate water, waste management, garbage and housing conditions (Caprara et al .125). During this study, it was found that the drinking water often became a mosquito breeding ground. The community did not have consistent availability to clean water. Residents were forced to purchase water from street sellers and horse drawn carts that were often not stored safely. Improper lids and insect-barring screens allowed the mosquitos to contaminate the water, leading to infections (Caprara et al. 131). Without the resources to create a system to protect drinking water and dispose of waste water, infections run rampant causing communities to fall ill.
Absence of necessary governmental support leaves a mark on communities. Investment in public services for people living in poverty is discouraged by social inequalities, as these inequalities lead to unequal healthcare access, social exclusion and lack of political interest in improving problems (Castro et al.). These nonexistent public services include public healthcare resources. Communities may have no access or scarce access to healthcare, and they might not be able to afford it, or be able to travel to it. Because of this, social class is linked to how sick a person gets. Marginalized groups like these tend to get sicker because it is difficult to get medical treatment. Early symptoms of dengue fever may not be recognized, leading individuals to seek care much later than other populations (Chang et al.). This is a stark contrast to wealthier individuals who have public health services readily available and are able to get a diagnosis and receive treatment sooner, preventing dengue from having serious effects.
Prevention Strategies
Governments and health officials did not always take a “hands off” approach when it came to dengue fever. During the 20th century, strides were taken to eliminate the disease. These projects focused mainly on reducing the population of A. aegypti. Efforts in South America were the most successful at this, and by the mid 1900s, Brazil and Bolivia had nearly eradicated the mosquito. This was only possible through planned preventative measures that were put in place regardless of the socioeconomic status of a community. Campaigns focused on procedures such as checking water containers for larvae and treating common breeding locations with oil. However, when pesticides were introduced, health officials dialed back on the original methods and turned their focus onto the use of DDT. While this worked for a time, it was ultimately unsuccessful. New serotypes evolved that were resistant to DDT and instead of shifting back to old preventative strategies, efforts slowly reached a halt. With no vaccine developed and no governmental support, communities were left to fend for themselves without proper tools to effectively stop the spread. As the 20th century came to a close, the Americas had been completely repopulated with A. aegypti and dengue fever was free to spread (Castro et al.). As dengue fever’s geography expands and infection rates rise, public health concerns are growing. Countries are paying more attention to this often neglected disease. As of March 2024, Puerto Rico declared dengue fever a “public health emergency”, as it is one of many countries facing record breaking numbers (Hernandez). However, public health experts have yet to reach a consensus on how to treat this. Some have suggested that communities can continue to deal with it on their own but this perspective takes away from a greater responsibility by placing blame on the individual. Oftentimes, blame for problems such as infectious disease will be placed on individuals or certain communities, instead of the root cause of the problem. Blame is also more likely to be placed on underserved areas (Farmer 188). The root cause of dengue’s expansion actually lies within climate change and the end of vector control programs. Currently, the rise of vaccines has moved attention away from active prevention strategies and onto mostly laboratory research. Governments lack incentive to deal with dengue fever, and the harshest consequences are suffered by marginalized groups (Castro et al.). In order to combat dengue fever, a combination of defense strategies must be implemented. Community education, active tracking of cases and early outbreaks, and risk maps as well as laboratory efforts should be put in place (Chang et al. 95). Until these changes are made, underserved communities will not only be blamed for the spread of dengue fever, but will continue to suffer from higher numbers of infections as well.
Conclusion
Dengue fever in underserved urban communities results from the interaction between biology and social elements such as a poor physical and socioeconomic infrastructure. Poor infrastructure will affect mosquito spread by ignoring problems related to overpopulation, water management, housing and healthcare accessibility. When low income communities are dismissed by their governments, these issues only worsen. Controlling dengue fever is only possible if communities are provided with the tools they need. As global warming increases dengue fever’s territory and infection rates, it has never been more important for action to be taken. Active vector control methods that address the biological and social aspects of this disease hold the key to stopping the spread.
Works Cited
Caprara, Andrea et al. “Irregular Water Supply, Household Usage and Dengue: A Bio-social Study in the Brazilian Northeast.” Cadernos de saude publica, vol. 25, Suppl 1 (2009), pp. S125-S136. doi:10.1590/s0102-311×2009001300012.
Castro, Arachu, et al. “Social Inequalities and Dengue Transmission in Latin America.” Plagues and Epidemics, edited by D. Ann Herring and Alan C. Swedlund, Routledge, 2010. pp. 231-249.
Chang, Aileen Y, et al. “Social Justice, Climate Change, and Dengue.” Health and Human Rights, vol. 16, no. 1, 2014, pp. 93-104.
Cromar, Lauren, and Kevin Cromar. “Dengue Fever and Climate Change.” Springer eBooks,
2013, pp. 167-91. https://doi.org/10.1007/978-1-4614-8417-2_10.
“Dengue Areas of Risk Around the World | CDC.” Centers for Disease Control and Prevention,
21 Sept. 2023, www.cdc.gov/dengue/areaswithrisk/around-the-world.html.
Desjardins, M. R., et al. “Knowledge, Attitudes, and Practices Regarding Dengue, Chikungunya, and Zika in Cali, Colombia.” Health & Place, vol. 63, 2020, doi:10.1016/j.healthplace.2020.102339.
Farmer, Paul. AIDS and Accusation: Haiti and the Geography of Blame. U of California
P, 1992.
Farmer, Paul. “Social Inequalities and Emerging Infectious Diseases.” Emerging Infectious
Diseases, vol. 2, no. 4, Dec. 1996, pp. 259-69. https://doi.org/10.3201/eid0204.960402.
Gloria-Soria, Andrea, et al. “Global Genetic Diversity of Aedes aegypti.” Molecular Ecology, vol. 25, no. 21, 2016, pp. 5377-5395. doi:10.1111/mec.13866.
Hernandez, Joe. “Here’s What to Know About Dengue, as Puerto Rico Declares a Public Health
Emergency.” NPR, 27 Mar. 2024, www.npr.org/2024/03/27/1241210938/dengue-puerto-rico-public-health-emergency-facts-disease.
Heymann, David L. “Social, Behavioural and Environmental Factors and Their Impact on
Infectious Disease Outbreaks.” Journal of Public Health Policy, vol. 26, no. 1, Apr.
2005, pp. 133-39. https://doi.org/10.1057/palgrave.jphp.3200004.
Kularatne, Senanayake A. M. “Dengue Fever.” British Medical Journal, vol. 351, 2015.
JSTOR, https://www.jstor.org/stable/26521869. Accessed 5 May 2024.
Messina, Jane P., et al. “The Current and Future Global Distribution and Population at Risk of Dengue.” Nature Microbiology, vol. 4, no. 9, 2019, pp. 1508-1515. doi:10.1038/s41564-019-0476-8.
“Serotypes and the Importance of Serotyping Salmonella.” Salmonella, CDC, 9 Sept. 2022, www.cdc.gov/salmonella/reportspubs/salmonella-atlas/serotyping-importance.html.
Whiteford, Linda M. “The Ethnoecology of Dengue Fever.” Medical Anthropology Quarterly, vol. 11, no. 2, June 1997, pp. 202-223. https://doi.org/10.1525/maq.1997.11.2.202.
Acknowledgements: Thank you to Dr. Susan Tanner for introducing me to medical anthropology!
Citation Style: MLA
